Midwifing the Portal Door
Midwifing the Portal Door
by Sister MorningStar
(First published on Midwifery Today)
Not all babies live. Not all wimyn die with their uterus. Not all mothers survive childbirth.
These are hard truths to bear. Hard truths for the family, community, and world to hold.
But truths set us free and help guide us to deeper understanding and reformation.
I know these are hard stories to hear, but there is help and healing and learning in the
stories. I pray you can discern that. I also have created guides to help develop our skills in
serving the psycho-social-emotional-relational-spiritual needs of the at-risk mother and
the support persons who care about her. First the Herstories, where fact and information
blend with feeling and the soul.
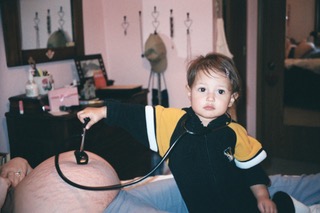
Sally wrote me asking if she could come to The Holyland for a healing. Sally had a
handsome, quiet, observant toddler and a Swedish husband. She was womb-full with a
third child, albeit in the early weeks. They borrowed a car, drove three hours to reach my
cottage in the woods, and Wilhelm gave some private time to me and Sally. They would be
moving in just a few weeks to seek new employment and a protected place to birth. Sally
was planning another freebirth. Her first birth was a homebirth transfer that ended in
birth by knife for her son. Her second child—her first daughter—was stillborn in the sacred
space of their home. A saintly neighbor named Anna came straightaway to comfort, clean
up, make prayers, and companion them as the necessary calls were made. Sally let a quiet
tear fall from her cheek as she told me her birth stories and shared the few photos she had
of her daughter, Malou. Sally felt she had received such grace, support, love, compassion,
and heavenly reassurance in her grieving journey. She had a natural and humble respect
for the unknown future of the birth and baby she now carried. Mostly, she was joyful and
excited to be cradling new life. She longed for purity and sacred prayers to accompany her
journey into this new mystery.
Wilhelm returned and the family circled in my little cottage with what seemed like a divine
halo around them. They were radiant, quiet, and loving to one another.
“We are no strangers to death, Sister.” Wilhelm spoke slowly with soft eyes. “We have lost
aunts, grandparents, and others. We know life fades. Life holds these truths.”
Wilhelm taught religious philosophy around the world. I asked him to tell me about
meeting Sally. He told me about their meeting in a European coffee shop.
“We started a conversation that day and we are still having it.” He smiled and took Sally’s
hand while the golden son sat quietly on his father’s lap and looked at his mother.
We made prayers and healing ritual together. I secretly determined to gather some of my
calmest, most powerful wimyn and journey to Kansas City to offer a private Village
Prenatal (1) for Sally. There were 10 days before she moved. I worked and prayed with
diligence. Two of my daughters who had birthed in power agreed to meet me there. Sally
was speechless with gratitude. She gathered two other wimyn to join us. A new mother
who had birthed in power, and Anna, a womyn of devotion and mother of many children
born at home. I brought my music maker, songs in my heart, talking stick, anointing and
massage oils, altar icons, power stories and chocolate. As of old, the wimyn gathered.
Unspeakables filled the afternoon. Sacred space for joy and sorrow and hope was reborn.
Anna announced her new pregnancy. A beautiful surprise! She and Sally would both be
due in September. Like Elizabeth and Mary, they made promises to one another. We
feasted on healthy, wholesome foods and sipped nourishing teas. Our goodbyes are still a
treasured echo in my mind.
Sally found a secure place to birth at home after months of travel. She made her nest. She
birthed her second daughter in the light of candle and under the sky, resounding with
exclamations of joy and triumph. A live daughter returned to Sally. We, her elephant
circle, knelt before our altars 1000 miles away and sang out: Her splendor reaches far
beyond the Heavens! May the name of Sally be praised! From the rising of the sun to its
setting! May the name of Sally be praised! (2)
Ellen was pregnant with new life as I prepared to leave on my mission trip to Mexico. It
was baby number six. The last baby had been born at home with anencephaly. Ellen sang
and held this holy child for 11 hours before he slipped away in his mother’s arms at home.
It was time to plant autumn bulbs and time for new hope.
I told Ellen, “Together we will see these flowers bloom when I return!”
“Maybe,” she responded.
Ellen birthed the night before I flew back home. One of my colleagues picked me up at the
airport wearing black. The funeral was to be the next day. The baby was born at home.
This child was microcephalic and Ellen died within moments of seeing her son. The
midwives with her grieved with the family and community. We buried a mother and baby
that day with broken hearts and searching spirits. During her pregnancy, Ellen had told
her parents and siblings, “I will not bury another baby.” They embraced us saying, “Thank
you for loving Ellen. We knew. There was nothing anyone could do.”
It was after the loss of Ellen that I created the assessment tool, “Maternal Loss Risk
Assessment” (3).
I was in San Miguel, Mexico, helping at a little maternity hospital that championed serving
the poor from surrounding villages, when Maria arrived with her husband, mother, and
several sisters. The night sky held many bright stars as I walked on the roof for fresh air
and to welcome the labor that was progressing quickly for this experienced mother. I
knew the staff would call me soon. I sang the songs and made the prayers as of old and as
was my nature.
The family was a bit anxious and glad to be with us. Their home in the village had no
running water and the few cars were not always quickly available. I looked into their
concerned eyes and kept my focus on the mother, who also appeared scared.
She had not been feeling well for some time. She had not felt her baby move all day. The
routine vital checking proceeded with increasing concern. A surgical birth was quickly
agreed upon. I prepared to enter the theater and be the one to hold her hand. The baby
was born lifeless. The surgeon closed the mother’s weeping womb. Wet eyes filled the
room. I kept my fingers on her pulse which was erratic. The anesthesiologist announced,
“We are losing her.” The surgeon did not want to open her back up shaking his head that
there was nothing more he could do.
Everyone pleaded with the Gods. The nurse held her tray like a frozen statue. The
pediatrician jumped up on the surgical table vigorously giving CPR. The lifeless baby lay in
a warmer with the blanket over his face. I held the hand of Maria, which was strapped to
an arm board. I whispered in her ear. I spoke gently to her soul. I felt the pulse go rapidly
up and begin to fade. She slipped away under my fingers, our prayers, the stars.
I supported the staff as they processed down the hall to meet the family in waiting. With
downcast heads and heavy hearts, we reported our failed attempts to save baby or
mother. I went to the garden and got a flower to put in the hands of the baby before
bringing the family in.
One of the sisters had tears in her eyes and spoke quietly to me. “I’m scared to have a
baby. This is my second sister who has died this way.” The death report for both her sisters
listed eclampsia.
We need a village caring about mothers, not just hospitals that handle emergencies. We
need wise wimyn in the village who carry the wisdom of ages and some modern
knowledge that integrates the body/mind/soul connection. Maybe there are some simple
ways we, as a caring community, can help. Sometimes it is the soul that dies first.
“It was harder to watch her spirit die 10 years ago than it was to bury her body today,”
Hanna tells me as the family and community mobilize to help care for the remaining
children, including her sister’s newborn baby.
The hospital donated a one-year supply of formula. I wondered about cross nursing (4)
because there were several sisters and in-laws with new babies, and an ample supply of
breastmilk. Even a grandmother can re-lactate to help an orphaned newborn. I was raised
hearing my mother recite this part of Henry Wadsworth Longfellow’s poem/ballad,
“Hiawatha.” I recited it to my daughters. I never see a newborn’s wide eyes under a night
sky that I do not begin the recitation. I am comforted to know that, even as a grandmother,
I can nurse an orphaned baby if her life depended on me.
By the shores of Gitche Gumee,
By the shining Big-Sea-Water,
Stood the wigwam of Nokomis,
Daughter of the Moon, Nokomis.
Dark behind it rose the forest,
Rose the black and gloomy pine-trees,
Rose the firs with cones upon them;
Bright before it beat the water,
Beat the clear and sunny water,
Beat the shining Big-Sea-Water.
There the wrinkled old Nokomis
Nursed the little Hiawatha,
Rocked him in his linden cradle,
Bedded soft in moss and rushes,
Safely bound with reindeer sinews;
Stilled his fretful wail by saying,
"Hush! the Naked Bear will hear thee!"
Lulled him into slumber, singing,
Ewa-yea! my little owlet! (5)
Evelyn died weeks after holding her 8-year-young daughter who took her last breaths in
her mother’s arms. Evelyn’s family knew she died of heartbreak, leaving other children
ranging from three to sixteen. But that is not what her death certificate said.
Ivy had twins. One lived. One didn’t. She struggled to stay and mother her other six
children. “If the baby didn’t need my milk, I wouldn’t stay. The other kids will be fine. I wish
I could be with my Amelia,” she told me over and over. When Ivy died unexpectedly years
later, just as the last child was old enough to “make it on her own,” those of us who knew
her secret daily wish to one day be with that sky child, felt a sword of grief pierce our
hearts and a shared happiness that she was getting her wish. Ivy had written ballads about
her sky baby and birth and the glory of heavenly angels who accompany us. We sing her
songs to this day. In her honor and to honor the power of such brave wimyn who birth and
serve birth.
Offering Village Prenatals returns dignity and connection to a birthing mother and her
community. It has nothing to do with being medical and everything to do with supporting
and feasting and listening and celebrating the holy state of Motherhood. It serves with
humbleness those who carry our future with bravery—however and wherever they plan
to birth. It has the potential of building a community who can show up when the outcome
of birth leaves a shadow of sorrow on the lives of a womyn with empty arms, a family
without a mother, a mother with serious blood loss, as well as the inevitabilities of
elderhood that challenge us all if we live long enough. We can create healing circles and
meal trains, organize older child outings, help with laundry, feed the dog, and make the
prayers. We can learn to work with a womyn’s family to co-ordinate extra help or work
temporarily like a family for a womyn in isolation. For this reason I created the
“Assessment Guide,” which helps build the support team for a longer, more demanding
recovery time.
What about hemorrhage? Excessive blood loss (EBL) in second or third stage leading to
transports and transfusions brings a mother too close to the portal door between the
worlds and sometimes carries her through it. If she also loses her uterus in the attempt to
save her life, or if she has prolapse that leads to hysterectomy later in life, she is facing
difficulties for recovery that deserve a community of loving care, not just medical
treatment. In a world of “google the answer,” we can, instead, share our knowledge and
experience and pool our care and resources to offer human contact that knows how to
respect privacy as well as move into action. Wimyn who gather have done this from the
dawn of time. We can too. Gather the wimyn.
Carol’s baby’s heart stopped beating at about 26 weeks in the womb. I was with another
mother about to birth when I got the panicked call from Carol’s sister (6). When she
started bleeding and went to the nearest hospital, an ultrasound was performed that
confirmed “fetal demise” and a breech position. The hospital had a policy of “no vaginal
breech.” Although the lifeless baby was starting to emerge, Carol was rushed to the
surgical theater for a cesarean, according to protocol. She was given general anesthesia.
By the time I reached the hospital to meet Carol and her family, they shared a mixture of
emotions, including shock, anger, and sorrow. Carol was told under no circumstances
should she attempt a vaginal birth in the future due to the type of incision made and the
placenta accreta they removed.
It took months of extra home visits to unravel and find answers to their mountain of
questions. Normally a very cooperative and faith-filled multi-generational family, they
became demanding, resistant, and distrustful of the authorities who had treated them
with such disrespect and disregard to their needs and wishes. They wanted their baby,
which was taken to the hospital morgue and sent to autopsy. The wait was unbearable.
They called every day.
We worked with the county coroner and county assessor to create a plot on their land
where the child could be buried according to their traditions. The result of the autopsy
was “cause unknown,” a conclusion my attorney has told me is about 60–80% of stillbirth
autopsies. Due to the estimated gestational age, the baby required a death certificate and
medical report. All of these legal, yet incomprehensible, requirements unraveled the
normally steady, calm nature of the family.
I attended the private, quiet, home burial. It was the first time Carol got to see her
daughter. Her husband, sister, and small family community were present. She asked if I
would help her look at her baby. Before we uncovered the face, I told her what we might
see and how her heart would see things differently than her eyes. I told her there was no
hurry, that we could take all the time we needed and stop at any moment. I told her she
could also look over every finger and toe and part of her baby she wanted, for as long as
she wanted. It was her baby. Carol took her time. She marveled over every inch of her
baby. In the field that day, under the blue sky, we embraced baby and covered her with
our love, our songs, our tears. We buried her little body with sacred prayers. Carol began
to heal. We all did.
The next year Carol birthed a live child triumphantly in her bathtub. Her greatest sense of
victory was the birth of her healthy placenta, whole and robust. She held both baby and
placenta in her arms and demanded the phone. She called the hospital and left a message
for Dr. ________. “I have in my own hands a live baby and a healthy placenta. You have no
right to tell me or any womyn what we can do.”
I used to think I was a midwife. Then I learned what other people define as a legitimate
midwife and I thought I wasn’t a midwife. Then I became a storyteller of the greatness of
the wimyn around the world who welcomed me into their lives for first and last breaths.
Then I realized one can’t midwife the sacred portal door between the worlds and not be a
midwife.
Don’t worry about what you call yourself or what other people call you. Gather the wimyn.
Notes:
1. Read can read about Village Prenatal and how to create one by searching MT archives
and visiting my website: sistermorningstarl.com
2. Anna also birthed another daughter that September. Quietly, humbly, and calmly at
home.
3. Maternal Loss Risk Assessment Handout is provided with this article or you can write to
me for a download: sister@sistermorningstar.com.
4. Indigenous people and people of old give an orphaned newborn to a newly-birthed
mother to nurse.
5. Henry Wadsworth Longfellow. 1855. From “The Song of Hiawatha, III. Hiawatha’s
Childhood.” www.hwlongfellow.org/poems_poem.php?pid=277.
6. The mother I was with gave birth to a daughter on the birthday of her twin daughters.
Baby number 5. “I guess I will be making three birthday cakes next year,” was the first
full sentence she made as you held her precious baby girl. “As well as three Sunday
dresses to match.”
7. Carol used homeopathic hydrastis, along with food, as medicine to help avoid a repeat
complication with placenta.
Sister MorningStar has dedicated a lifetime to the preservation of instinctual birth. She
birthed her own daughters at home and has helped thousands of other women find
empowerment through instinctual birth. She is the founder of a spiritual retreat center and
author of books related to instinctual and spiritual living. She lives as a Cherokee hermitess and
Catholic mystic in the Ozark Mountains of Missouri. Visit her on the web at:
The Power of Women: Instinctual Birth Stories: When women embarked on their journey into
womanhood and motherhood, stories from their grandmothers, great-grandmothers and
ancestors came forth through songs, stories and what appeared as mythological tales. Upon
hearing these stories, women became empowered to do what all women from which they came
were able to do: give birth instinctually.